Top 10 Biggest Hospice Mistakes
In 20 years of serving Hospice we’ve seen a lot of mistakes. One was the CEO who bought a cow for the Hospice. Another was the CEO who asked her CFO to create a 10-year budget. Sometimes you don’t know whether to laugh or cry . . . or just shake your head. Fortunately, nearly all mistakes are fixable–or you just live with them. But some mistakes can be fatal to an organization. We want to prevent that. And for many Hospices, we have. For many others, we’ve shared our experiences and helped prevent them from going down painful roads. Yet, others, particularly large organizations, can’t be taught. It’s not that they’re not smart. To the contrary, they’re very smart. Too smart for simplicity. We’ll share ten dangers we see every day. It’s certainly not a comprehensive list and it’s probably not in order. We hope it will help you.
ONE
Relying on a Budget rather than a Model
Budgets hurt Hospices. Budgets hold them back. They rob time and focus from truly important things. Here’s why:
- Budgets are Almost Instantly Outdated – Static Budgets often lose their comparative value with fluctuations in patient volume. Any increase or decrease in census will cause material overage or underage in census-sensitive areas. Often the budget will have to be “revised.” Also, static budgets are normally all but ignored by the end of the year! All focus is on “next year’s budget.”
- Budgets are a Colossal Drain of Time and Energy – Most Hospices spend tremendous time (months) creating the budget. It is truly one of the most wasteful uses of resources and energy in most Hospices. A budget is usually outdated within the first months unless census approximates the budget.
- The Idea of Budgets is Negative – Budgets do not excite people. They are not motivating. They are the opposite. Budgets are limiting, truncating, and stiff. The term budget doesn’t stir the imagination and garner much enthusiasm or cheers. A “Model”, or whatever term you want to substitute, is alive and flexible. A new name also accommodates the best ideas.
- Budgets Offer Little Comparability or Perspective – Traditional budgets are difficult to compare to other similar organizations. Few aspects of budgets lend themselves to comparison to gain the much needed perspective that separates true Hospice professionals from amateur Hospice leaders.
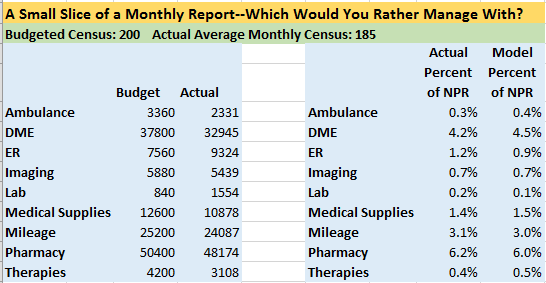
When you manage to a Model you avoid all of the negatives of a budget and you get far better management reports. Look at the comparison below. Which is simpler to manage with?
When you drop your budget and manage to a Model and you’ll see
- The Model is always based on Current Census – The Model automatically adjusts every category based on Net Patient Revenue (NPR) which is derived from census. You are always comparing “apples to apples” with the Model approach. In accounting, you have two types of variances, volume variances and efficiency variances. The Model eliminates the volume (census) variance and all that remains is the efficiency variance. With a traditional budget, these two variances are “combined” making decisions drastically more difficult.
- The Model Establishes Standards – The Model forces a Hospice to establish financial and operational Standards. Areas include: caseloads, weekly visits, visit durations, costs parameters, et cetera. These Standards apply regardless of fluctuations of patient volume!
- Transparency – The Model based on NPR creates the immediate transparency that so many organizations seek. Percentages are widely understood by most people. Because the Model uses percentages as the common unit of financial measurement for all areas, anyone that is familiar with the Model amounts could easily evaluate the performance of any department or area. This would mean that if the Model were taught throughout a Hospice, ANYONE, from staff member to Board of Director to volunteer, could judge financial performance.
- Comparability – Because the Model is constructed on a Percentage of Net Patient Revenue basis, a common unit of measurement, results are easily comparable to other Hospices. In fact, each line item is comparable so, a Hospice is not even limited to comparing grand totals or broad categories. Again, perspective and insight into the overall Hospice world separates the Hospice professional from the amateur Hospice leader.
- Once Established, the Model takes Little Time to Maintain – The Model is a perpetual system. It continues to be used indefinitely until the decision to change it is made. There is no need for months of effort to create something new. A Model can be changed in minutes, if needed.
- The Model is Flexible – If the Model needs to be changed it can be altered in minutes to accommodate the new direction. It is not the alteration of the Model, mechanically, that is what is time consuming. It is the “what” and “how much” questions that require much mental work. However, this is exactly where we should be spending our time, thinking of improvements rather than thinking about the mechanics of measurement.
- The Model is More Easily Understood – People “get’ the Model concept. It is that simple! They understand easily that the “pieces must work together” by the mere mention of the word Model.
- The Model Still has Static Goals – A well-developed Model will have static or established goals. These are similar to the goals in the traditional budget in that normally annual goals are created. The Model establishes goals as well. However, the goals or targets pertain to things like ADC, Model %s, productivity measurement, et cetera. It does not pertain to static dollar amounts for each area of the Hospice. Also, we recommend the use of the term “goal” rather than “target” or another term. Goal has a less negative connotation.
- The Model can produce a Traditional Budget when one is Needed – Need a budget report for the United Way or the Board of Directors that does not understand a Model approach? The Model System can produce an annual budget in minutes as the current Standards are projected into the next twelve months. These amounts can be uploaded via F9 into your accounting system to produce a traditional budget report.
- The Model becomes a Forecasting Tool – Relating to the point noted above, the Model can be used as a forecasting tool. A Hospice can change the Standards in the Model and project operational performance into the future. The Model becomes a decision support tool.
Now you may be thinking, “We’re smart people here. We’ve got a crack accounting team and we’re not afraid to manhandle a budget.” But, it’s not about you. It’s about the people who need good information to manage with. Smart people love complexity. Wise people love simplicity. Management reports are for managers, and managers don’t have time to mentally readjust every line item as census shifts. Do the right thing. Kill your budget.
TWO
Lack of an intentionally designed visit-structure (with IRMs)
Could your Hospice’s CEO do a routine care visit today? Can your organization’s marketer describe how a visit from your organization differs from a visit from any other Hospice in your community? And here’s the hardest question: What’s the variance of visit quality between your best nurse and your worst nurse. (Ouch.)
We call it visit structure. It’s the basic widget of Hospice. It is one thing to have a visit structure designed. It is quite another when you can pull ANY clinician at random and have the person recite as well as demonstrate your visit system!
The implications of THE VISIT are far reaching from quality of care to financial. Few Hospices have intentionally designed the visit for each discipline. The primary reason a Hospice should have a defined visit structure is to decrease the “variability of care” from one clinician to another. There is great variability of quality among Hospice team members and this has gotten our movement in trouble. A visit structure is only 30% prescriptive. The remaining 70% of the visit is dependent upon the clinician’s independent judgment. Thus the structure supports helps clinicians especially when they are tired. In addition, a structure helps a Hospice brand it services. By using it, we guarantee that things will not fall through the cracks or be overlooked.
Visit structures have to be memorized, because no practice can be operationalized unless it can be remembered. But aren’t hard to learn if you use IRMs—Image Recall Mechanisms. We believe visual images with attached meaning can be intentionally crafted for practical use. Through the use of IRMs™, images can be fixed in the minds of viewers, meaning can be attached and mechanisms can be positioned to facilitate recall. For example, if the nurse has a little sticker with this image:

Would she remember the “eye level-lean-in” component of the visit? Every time. So, we attach and strategically place an IRM to every component of the Visit. Is this easy to do? No, it takes work. Does it result in vastly improved overall visit quality? Of course.
Here’s how it works:
- Design your visit structure (including each task associated with each phase of the visit). Remember, it’s all about the “feeling.” Mentally put yourself in the patient chair. Consider how patients and care-givers feel during every aspect of the visit. Start with the pre-visit, consider parking, entrance, sanitation, documentation, the exit—everything. You’ll want a written visit structure for every kind of visit. This is so important we’ve created a visit structure guide and videos on the subject.
- Train your staff in the habits of doing every visit according to your Standards. This would include use of your point-of-care devices and documentation. The visit is where documentation takes place…and it has to be perfect. 100% is the only acceptable Standard in this area (or really any other area)! Anything less must not be tolerated. But this will only happen if every clinician is working according to a well thought-out visit structure. Make structures simple and do not tolerate deviation…that is unless you want an unpredictable, unsatisfying and sloppy care experience. Failure to do this is the main reason many Hospices are in trouble and why our movement’s reputation has been damaged. We owe it to our patients and families to examine EVERY aspect of the care experience. You want to create an extraordinary experience for every patient, every time.
THREE
Relying on Donations to Break Even
Many Hospices are one public relations disaster away from bankruptcy. If your organization is reliant upon community support you may not weather the storm. Don’t think it can happen to you? Google “Hospice closing.” It may not be a bankruptcy, but a Hospice that is not self-supporting is a Hospice at risk. Every year we see multiple Hospices calling us too late. Usually they don’t close. They are absorbed by bigger stronger organizations. And the bigger the organization, usually the worse for the community.
Go ahead, raise all the money you can through donations, but operate your Hospice as if you receive ZERO support from the community.
Andrew says:
We are on a mission to keep as many not for-profit Hospices from tanking. This directly relates to profitability. So at the risk of staying in trouble, let’s destroy many of the not for-profit ideas that plague Hospice. Frankly, I think that many for-profit players have it right from a business standpoint…and not for-profit’s need to take some lessons. With this said, there are bottom feeders in both the not for-profit and for-profit domains that need to be wiped from the Hospice slate. From an objective standpoint of seeing hundreds and hundreds of Hospices, I can say unequivocally that the majority of truly creative “management” innovations in the Hospice movement have come from for-profit Hospices. Now don’t get me wrong, many for-profits have plenty to learn from not for-profits as well. However, the management practices of many for-profits should be emulated. It is interesting to note how many of the really, really successful Hospice CEOs in the for-profit domain have come from not for-profits. The fact that the ADC size of for-profit Hospices is growing, sometimes at phenomenal rates, tells us that they know something about managing Hospices. Many times, for-profits are even among the most spiritual Hospices with healthy cultures that know how to balance purpose and profit. There is no monopoly on best practices by either for-profit or not for-profit Hospice organizations.
If I am helping to build a Hospice business platform, I construct the operational methodologies with basically the same components, tweaked for overarching philosophies of who is paying for the assistance. Community Support does not even come into the picture for me. Deborah Dailey trained me well in this regard as she refused to operate a Hospice on the kindness of others. My directive was that Community Support didn’t exist…and that I MUST learn to operate a Hospice only on earned dollars from Medicare, Medicaid, Commercial Insurance and Private Pay.
Being a not for-profit organization is not an excuse for being wasteful. In fact, it is the just the opposite. A not for-profit must be even more prudent regarding its allocation of resources.
Here are some common, confused and misplaced Not-for-profit Ideas:
- Hospices need Community Support in order to operate.
- Not-for-profits shouldn’t make a lot of money.
- Not-for-profits care more about patients and families.
- For-profits have some mystic “advantage” over not for-profits.
- For-profits skimp on care.
- Not-for-profits provide higher quality care.
- Not-for-profits can’t pay their staff’s well.
- Volunteers prefer to give their time to not for-profits.
- “If we are highly profitable, Medicare is going to cut our rates.”
- “If we are highly profitable, people won’t give.”
- Not-for-profits Boards of Directors are more committed than FP Boards.
All of these ideas are false. Yes, you can find specific instances for each of these statements that is contrary and “weenie-out” to escape the overall reality. However, if ONE organization deviates, it proves that the view does not necessarily apply to the whole. Again, we find ourselves in the world of the outlier…
Many non-profit Hospice organizations think they can’t or shouldn’t operate as a business. They’re sustainability strategy is, “Do we feel lucky?”
FOUR
Your In-Patient Unit
We encourage In-Patient Units, in certain circumstances. There are at least three strong reasons to have a Hospice In-Patient unit:
- Mission Fulfillment – It should be your goal to serve everyone that could benefit from Hospice services in the market you have chosen.
- Competitive Edge – If your Hospice has one and the others don’t, you have an edge. Patients and families love these units.
- Increased Revenue Opportunity – Properly managed units provide good financial results.
But, don’t build an IPU that you cannot afford. IPUs are closing Hospices. Wrecking organizations. In 2015 we saw two clients saddled with IPUs they couldn’t afford. Both clients eventually folded into larger Hospice organizations. While under the right circumstances some IPUs make money, it’s rare. If you have an IPU you must exercise constant vigilance over its costs.
Here’s the rule: IPUs losses cannot exceed 4% of your net patient revenue for routine care. This pre-supposes that your routine care Model gives you a 14% return on routine net patient revenue . . . which, of course, is The Model that MVI teaches.
The Three Major Factors of IP Unit Financial Success
- Design of Unit/Location of the Unit
- Clinical Leader
- Bed Management
- Staffing within the Model
- Control of Patient-Related Costs
- Clinical Practices of Unit Physicians
The #1, most important, super factor of an IP Unit’s success is the Leader of the Unit! Never overlook this! This leader needs to be a great relationship builder, salesperson, aggressive (calling the health systems on Thursday/Friday to fill the unit up before the weekends), understands “heads in beds” and understands how to flex staffing as needed.
Inpatient Unit Financial Problems
There are a lot of Hospice IP units and more being built or implemented. Why? Many have figured out how to make IP units financially viable, understand their importance with the aggregate CAP and how much communities appreciate them. However, there are a growing number of Hospice IP units that are falling on tough financial times…through their own doing for the most part, with the median loss being around 14% of NPR of IP Unit revenue at the time of this printing.
Most of the problem is in staffing. There is a trend in Hospice IP units to reduce staffing ratios for RNs and CNAs to 4:1 and sometimes even less. Think about this. Where else in healthcare do you find these ratios? Consider what staffing is like in ICUs and Critical Care Units. Hospice units are often staffed at similar levels. The question is, “Is this the way it needs to be?” Or perhaps the better question is, “Is this the way we want our Hospice IP unit staffed?” The standard in Hospice IP units is one RN and one CNA per 6 patients, translating to 3 patients per team member, excluding SW and Chaplains. Less than 5:1 ratios for RNs and CNAs does not “pencil” very well. 5:1 works in “rare” situations. Some Hospices add additional staff when the census is at capacity, as the revenues generated can easily cover the additional positions. Spiritual Care and Bereavement are treated just as a Hospice would serve Nursing and Assisted Living facilities. A 12+ bed unit needs a full-time, devoted SW.
The other contributing factor is bed management. You must “design” your intake processes so that you keep the IP census at an acceptable level. This means weekend admissions, tracking nurses to identify ones who are not referring patients to the unit, evaluating your criteria, looking at how you have “trained” your referrals sources, et cetera. Do your clinicians really understand the value and benefits of the unit?
BEST PRACTICE: Your Hospice needs to find the average propensity of a clinician to refer to the IP unit and then design an “exception report” to identify clinicians who are not referring patients. ALL clinicians statistically should be referring a proportion of their patients to the unit based on need. If you discover that a clinician is not referring patients to the IP unit, you have a Lone Ranger! These clinicians basically are doing their own clinical practice and are dangerous on many levels. Just the fact that you are monitoring this will cause IP census to increase. We usually recommend that each case manager, within a 30-minute drive-time range of the unit, send a minimum of 4-5 patients to the IP unit every quarter.
ANOTHER BEST PRACTICE: Know the Magic Bed! The Magic Bed is the one that pushes your IPU unit to or past the breakeven point. You have to know that! And when that Magic Bed is empty, the whole Hospice organization should be alerted! C’mon, we’re dealing with the sickest people in your community. There’s certainly someone in your care who needs to be in that Magic Bed.
FIVE
Poorly Trained Marketers
(This section is not about Marketing, it’s about training the Marketer.)
Not all Hospices use marketers (or any of the many other names by which we call our sales persons). But to grow, you’ll need them. All literature and studies on Hospice marketing begin with the Hospice experience. We’ve been teaching that for years (read more about Visit Structures in this document).
Train the marketer as you would train a new nurse. The marketer must know the visit, the admission inside and out. The marketer won’t understand Hospice, and cannot manage the expectations of referral sources until she understands the visit itself. Every marketer should be certified in the visit as should everyone in your organization.
Let’s expand on the paragraph above. In 2017 we contracted with a 185 census Hospice in the mid-west to help them implement their Model. We started, where we always start, with standards and people development. Part of the process required everyone in the organization, from the CEO to the janitor, to certify on the visit. Certification involved performing a visit in their synthetic training lab and reviewing the video. It also involved a series of training videos followed by tests. During the certification process census began to grow. And grow. This organization was doing a lot of other things, and they had a great marketing staff, but as the marketers learned more about the visit and saw overall quality in the Hospice rise, census increase by 30%.
Let’s also train our teams to follow up with our referral sources. If we get a patient from a new referral source, we need to give regular feedback about that patient to that source. We have to make sure that source knows we delivered.
SIX
Personal Inspection of Work
Some of the best Hospices in the world were started by a Nurse in the 80s, working by herself, doing it all. It’s a common theme. That nurse builds the organization until it’s strong and profitable. She was the glue, and everyone reported to her, and she knew everything that went on. And then she retires. But the foundation was laid, and the Hospice continues to grow until they have more employees than they ever thought, but they’re still trying to manage the way we did 20 years ago.
Now we have systems. We can implement standards tied to our systems. And we can tie our standards to our compensation. When we link systems to standards and standards to compensation, we change the way our Managers manage. Our Managers become teachers, because they no longer have to check up.
This is where a typical Hospice’s Accountability system breaks down. IF our Accountability system is completely or near-completely reliant upon the supervisor, your system is not very robust. However, the personal inspection of work is still one of the essentials of a great Accountability system. The constraint of the human physical container is time and Energy. Therefore, when building a position, all work must be engineered to be completed within the constraints of time and Energy. For a sustainable job or position, it must be engineered so that all tasks can be completed to 100% of the Standard. This includes the personal inspection of work. A Manager should lead from the front. The Manager will get the behaviors they exhibit and the reward. A constant Management presence on the front line motivates people to do well. Again, this must be “built” into the design of a position.
Two systems to protect Managers from personal inspection of work.
- Incident reports with Essays. This is a relatively easy method of Accountability to implement and it is effective. Using documentation as an example, an RN fails to document a visit to the Hospice’s Standards. Upon detection (by Compliance or other), the RN must come into the office that day, fill out an Incident Report, sign it and complete an essay explaining how his or her lack of documentation impacted the team. You will get pushback on this initially. You will also get REAL insight into the behaviors of your team members. Some essays will be filled with excuses as to why they didn’t document to Standard. These are the weenies. You have to question whether they are fit to represent your Hospice. Other clinicians will take responsibility, which is exactly what you want! “I did it, I fess up. It won’t happen again.” You want people to take responsibility for their actions and to be grownups. This method of Accountability can be applied to many, many things.
- Compensation. Compensation is your most POWERFUL structural tool for addressing Accountability and creating healthy cultures/workplaces. People behave the way they are paid. This compensation can take the form of financial or non-financial rewards such as Emotional satisfaction or an increased inner sense of wellness. However, here the focus is financial. Before coming to Hospice, Andrew worked for a company that specialized in compensation systems. In his first Hospice experience, he implemented a performance-based compensation system for clinical staff. The result was a 100% increase in productivity, for all disciplines except one, and a 100% increase in the timeliness and quality of documentation. Compensation is the fastest way out of financial trouble and the fastest way to create a healthy Hospice culture. Why not let every paycheck become an automatic report card?
Every Hospice, yea verily, every organization needs accountability structures in place. And our systems can enforce them for us. Here’s a simple example
- Establish clear standards about documentation
- Teach those standards and certify on them
- Relieve your clinical managers from the task of checking documentation
- A designated person (sometimes it’s the on-call person when she not out and about) spot checks documentation to your organization’s degree of statistical comfort.
- Found errors are reports back to the clinician by email and copied to the clinical manager and the payroll clerk.
- The clinician has 24 hours to fix the problem and report back to the payroll clerk and the clinical manager
- If the payroll clerk doesn’t get that feedback, the clinician “misses out” on some designated regular bonus for 100% error free documentation in her next paycheck.
SEVEN
Poor Phone Interactions
The person (or machine) who answers your phone can undo a year’s worth of marketing efforts by your best marketer. The person (or machine) who answers you phone can cause non-physical pain to patients and care-givers. Care begins when the phone rings. But most Hospices don’t believe that. They believe people and referral sources are quite happy to talk to a machine. Are you happy talking with a machine? Do you look forward to calls to your credit card or wireless provider? So why do you emulate them?
As we move into the future, an increasing amount of the care we provide is going to be done via telecommunicative means. Phone interactions, emails, voicemail messages and texts are examples of modes of telecommunications. Each of these needs to be considered. Some may not be viable or best. But each needs to be considered. It is important to step back and notice how people in the modern world get their communications and use them if deemed to be beneficial. Therefore, as part of Sunny Day’s Model, we do not take phone interactions, or any interactions for that matter, for granted…nor do we assume that everyone knows how to create a satisfying customer experience via telecommunicative means. This short film will help to demonstrate some of the expected elements and qualities of Sunny Day’s phone interactions. The effective use of a phone or other telecommunicative device is a skill. And as we advance into the future, our ability to convey our compassion, care and competence will be increasingly through telecommunicative means.
EIGHT
Under-Utilization of Volunteers
We know of one Hospice who had a census of more than 70 patients a day and, until the last few years, had no employees. None. It was a total volunteer effort. Every clinician. The CEO. The CFO. And they’re still a largely volunteer organization. We know of another Hospice who has a waiting list for volunteers. That’s how Hospice was meant to be. What changed? A lot of things, but one of them is this: We don’t think we can recruit, train and utilize a volunteer force. We don’t believe.
Think about this: Hospice is the ONLY government program that mandates volunteerism. (It’s also the only government program that mandates spirituality. But that’s a thought for another day.) Andrew frequently says the Volunteer Coordinators in our Hospices are often the weakest managers. We need to recruit our Volunteer Coordinators just as we recruit our CEOs. If fact, your Volunteer Coordinators should have all the qualities of your CEO. The primary jobs of both are the same: To cast a compelling vision! We need volunteers making clinical visits, we need volunteers making phone calls, and we greatly need volunteers in the nursing homes! You don’t have volunteers because you don’t believe in volunteers. You don’t believe they can be managed (they can) and you don’t believe your organization can be a source of fulfillment to a volunteer. You can make it so.
NINE
Too Many Programs!
There are deep needs all around us. And, as Hospice people, we’re largely wired to help and serve. But which is better: To do one or two things REALLY REALLY well or to do many things poorly? More and bigger doesn’t always translate to more impact, more meaning. Often, “more” just complicates matters and, if there are efficiency problems, compounds them. It is better from multiple perspectives to do less well. Less is simpler. Complicated doesn’t work well. Simple does. Less is easier on the mind. Stress levels decrease. Less gives you better focus. As a Leader, I would be more interested in allocating resources to those things that are our core competence or vision than things that are peripheral. Outsource peripheral things, if they are needed at all. Stick to what you know. Bring laser beam focus to your competencies.
Andrew uses this analogy: A farmer with 500 acres of meticulously cultivated land will out produce (per acre) a conglomerate of 25,000 acres farmed with average intention. There is an inherent loss of efficiently when things get bigger. By virtue of size, there is inherently more to manage, more to break or go wrong…more to do. We all know that when we try to do too much and overextend, quality suffers and things are more apt to fall through the cracks. Energy levels are stretched. The same holds for our Hospice businesses. Farm less ground well.
(Side note about palliative care programs: Many Hospices want a palliative care program, and that’s fine. Just stay within your Model. Keep two things in mind every day when you move into palliative care:
- Limit palliative care program losses to 2% or less of your routine hospice care net patient revenue
- Watch your palliative care staff. They love their patients and want to hold them too long. They tend to hold on to their patients far past where they should really be in Hospice care. That’s not good for the patient and not good for the organization.)
TEN
The Wrong Passengers on the Bus
You’ve heard this one. It’s management lore and widely preached by every consultant in the world. Yet most organizations, especially the caring-professions struggle with it. It’s from the Jim Collins book Good to Great.
He says: You are a bus driver. The bus, your company, is at a standstill, and it’s your job to get it going. You have to decide where you’re going, how you’re going to get there, and who’s going with you. Most people assume that great bus drivers (read: business leaders) immediately start the journey by announcing to the people on the bus where they’re going—by setting a new direction or by articulating a fresh corporate vision. In fact, leaders of companies that go from good to great start not with “where” but with “who.” They start by getting the right people on the bus, the wrong people off the bus, and the right people in the right seats. And they stick with that discipline—first the people, then the direction—no matter how dire the circumstances.
We teach Hospice Managers to make two lists
- The “gotta-grow” list. These are A-List, high-performers that you want to nurture and grow. They will make your organization better and can take on larger challenges. They can reinvent your Hospice in a good way.
- The “gotta-go” list. These are people who are in the wrong positon or in the wrong organization. Some will wreck your system. Others will never “get it.” They can’t stay.
Top managers will make those lists. Today.


